Sep 19, 2022

IPPS Changes for FY2023
In the previous two parts of this four part series, we discussed the new ICD-10-CM diagnosis code changes and ICD-10-PC procedure code changes. For part three we will review the major IPPS changes for FY2023.
IPPS Changes Financial
On August 2, 2022, CMS published the Final Rule for IPPS (CMS-1771F) FY2023 IPPS Final Rule
Acute care hospitals that report quality data and that are meaningful users of EHRs will receive approximately a 4.3% increase in Medicare operating rates. Hospitals that do not submit quality data would lose 1/4 (-25%) of the market basket update (-25% of the 4.3% as above) This would be 3.225% for those not submitting quality data for FY2023. Hospitals that are not meaningful users of EHRs will be subject to a ¾ or 0.75%) reduction of the market basket for FY2023.
CMS is projecting that with the 4.3% increase and other changes to IPPS policies it will boost total IPPS payments in FY2023 by roughly $2.6 billion.
The CMS “New COVID-19 Treatments Add-on Payments” (NCTAP) will be paid through the end of the fiscal year (9/30/22) in which the PHE ends for all eligible products and new tech add-on payments for FY2022 unless extended by CMS. See https://www.cms.gov/medicare/preventive-services/covid-19-services-billing-coverage/covid-19 /new-covid-19-treatments-add-payment-nctap . CMS is revising the hospital and CAH infection prevention and control CoP requirements that require hospitals and CAHs, after the conclusion of the current COVID-19 PHE, to continue reporting on a reduced number of COVID-19 data elements. The revisions will apply upon conclusion of the COVID-19 PHE and continue until April 30, 2024, unless the Secretary establishes an earlier ending date.
There were no new changes to the Post-Acute Care Transfer Policy for FY2023.
Quality Measures
Also, in light of the COVID-19 PHE, CMS finalized adjustments to its hospital quality measurement and value programs. Specifically, for FY 2022, and continuing for FY2023, CMS will suppress (i.e., not use) most hospital value-based purchasing program measures. As a result, hospitals would receive neutral payment adjustments under the VBP for FY 2023. In addition, CMS will suppress all six measures in the Hospital Acquired Condition (HAC) Reduction Program performance for FY 2023. Hospitals will not be given a measure score, a Total HAC score, nor will hospitals receive payment penalty.
Lastly, for the FY 2023 Hospital Readmissions Reduction Program, CMS will suppress the pneumonia readmissions measure, and to exclude COVID-19 diagnosed patients from the remaining five measures.
Hospitals are required to report measures and meet the administrative requirements of the IQR program to avoid having their annual market basket update reduced by one quarter. The IQR also includes requirements to report electronic clinical quality measures (eCQMs) that align with the eCQM reporting requirements in the Promoting Interoperability Program. (Generated by provider’s E.H.R.) https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/ClinicalQualityMeasures.html
CMS is finalizing to adopt 10 new measures and refinements to two current measures (“Elective THA/TKA” and “Excess days in acute care after hospitalization for Acute MI”). See this link for description of these measures under “Hospital IQR Program https://www.cms.gov/newsroom/fact-sheets/fy-2023-hospital-inpatient-prospective-payment-system-ipps-and-long-term-care-hospital-prospective
Regarding Hospital Value Based Purchasing Program In Final Rule FY2023 CMS is:
- Suppress the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) and five Hospital Acquired Infection (HAI) measures, for the FY 2023 Program year;
- Remove the Patient Safety and Adverse Events Composite (CMS PSI 90) measure beginning with the FY 2023 program year. CMS continues to consider patient safety a high priority, but because the CMS PSI 90 measure is also used in the HAC Reduction Program, CMS believes removing this measure from the Hospital VBP Program will reduce the provider and clinician costs associated with tracking duplicative measures across programs.
CMS is also finalizing their proposal to revise the scoring and payment methodology for the FY 2023, like in 2022 program year such that hospitals will not receive Total Performance Scores. Instead, we are finalizing proposal to award each hospital a payment incentive multiplier that results in a value-based incentive payment that is equal to the amount withheld for the fiscal year (2 percent).
As a result of the above measure suppressions for the FY 2023 program year, CMS believes that calculating a total performance score (TPS) for hospitals using only data from the remaining measures, all of which are in the Clinical Outcomes Domain would not result in a fair national comparison. Therefore, CMS is finalizing to not calculate a TPS for any hospital based on one domain and to instead award to all hospitals value-based payment amount for each discharge that is equal to the amount withheld. CMS is also finalizing to calculate measure rates for all measures and to publicly report those rates where feasible and appropriately caveated. The agency is also updating the baseline period for certain measures affected by the ECE granted in response to the COVID-19 PHE and to make a few technical administrative updates.
For the Hospital-Acquired Condition (HAC) Reduction Program, CMS finalized their proposal to suppress CMS PSI 90 measure and the five CDC NHSN HAI measures in the HAC Reduction Program for the FY 2023 program year. CMS is finalizing proposal to apply that measure suppression policy to suppress certain program data from FY 2022, FY 2023, and FY 2024 HAC Reduction Programs; CMS is not finalizing our proposal to not calculate measure results or scores for the CMS PSI 90 measure for FY2023
Although CMS will not calculate or report the CMS PSI 90 measure results for use in the HAC Reduction Program scoring calculations for the program year, CMS will still calculate and report CMS PSI 90 that is displayed on the main pages of the Care Compare tool hosted by HHS.
Hospitals will not receive a Total HAC Score nor receive payment penalty.
For the FY2023 Hospital Readmissions Reduction Program (HRRP) 30 day readmissions, CMS is
- Resuming use of the Hospital 30-Day, All-Cause, Risk-Standardized Readmission Rate (RSRR) following Pneumonia Hospitalization measure (NQF #0506) and it will exclude patients with COVID-19 on admission, beginning with the FY 2024 program year;
- Resuming use of the measure above and modifying the remaining five condition-specific readmission measures to exclude COVID-19 diagnosed patients within 12 months prior to index admission from the measure denominators, beginning with the FY 2023 program year; along with using MedPAR data that aligns with the applicable period for FY2023. See https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program#:~:text=The%20Hospital%20Readmissions%20Reduction%20Program,the%20quality%20of%20hospital%20care
MS-DRG Changes
There were several changes involving MS-DRGs for FY2023. Below are the changes.
MDC 1: Nervous System
Laser Interstitial Thermal Therapy (LITT) codes were removed from the radiation therapy session and placed in the Medical Surgical Body Systems with Root Operation Destruction. LITT of brain and brain stem will now group to MS-DRGs 023, 024, 025, 026 and 027 for craniotomy and endovascular procedures
For clinical consistency with the other procedure codes describing the insertion of the stimulator generator, CMS is adding 24 ICD-10-PCS codes to MS-DRGs 252, 253 and 254, (Other Vascular Procedures with MCC, with CC, and without CC/MCC, respectively) in MDC 05 (Diseases and Disorders of the Circulatory System) effective October 1, 2022, for FY 2023.
CMS is also finalizing adding 108 ICD-10-PCS code clusters listed in Table 6P.3a in association with the proposed rule that describe the insertion of a stimulator generator, that is not differentiated by device type, and a neurostimulator lead to - 041 Peripheral, cranial nerve and other nervous system procedures with CC or peripheral neurostimulator, effective October 1, 2022, for FY 2023.
MDC 4: Respiratory System: CMS is reassigning cases reporting diagnosis code J80 (Acute respiratory distress syndrome) as the principal diagnosis from MS-DRG 204 (Respiratory Signs and Symptoms) to MS-DRG 189 (Pulmonary Edema and Respiratory Failure). This is due to the coding directive that acute respiratory failure progressing to ARDS is only coded to J80.
MDC 5: Cardiovascular System: CMS is finalizing proposal to remove procedure code 02UG3JE from the list for PTCA procedures in the GROUPER logic for MS-DRGs 231 and 232 (Coronary Bypass with PTCA with/without MCC) For Type 2 MI, requester said if I21.A1 is coded with PDX in MDC 05, DRGs 280-282 (Acute Myocardial Infarction, Discharged Alive with MCC, with CC, and without CC/MCC, respectively) is assigned. A type 2 myocardial infarction is not a true acute myocardial infarction. It will be assigned to MS-DRGs 266 and 267 (Endovascular Cardiac Valve Replacement and Supplement Procedures with and without MCC, respectively)
CMS is modifying the GROUPER logic to allow cases with the BAROSTIM NEO™ System (0JH60MZ with 03HK3MZ or 03HL3MZ) reporting diagnosis code I97.130 or I97.131 (Postprocedural heart failure following cardiac/other surgery) as a principal diagnosis to group to MS-DRGs 222 and 223 when reported with qualifying procedures.
CMS finalized the proposal to reassign procedure code 02K80ZZ (Map conduction mechanism, open approach) from MS-DRGs 246, 247, 248, 249, 250 and 251 to MS-DRGs 273 and 274 (Percutaneous and Other Intracardiac Procedures with and without MCC, respectively) in MDC 05.
MDC 7: Hepatobiliary system: Redesignate procedure code 0FC94ZZ (Extirpation of matter from common bile duct, percutaneous endoscopic approach) to an O.R. procedure and add it to the logic list for common bile duct exploration (CDE) in MS-DRGs 411, 412, and 413 (Cholecystectomy (open or laparoscopic) with C.D.E. with MCC, with CC, and without CC/MCC, respectively). This code had not been an “OR procedure” previously.
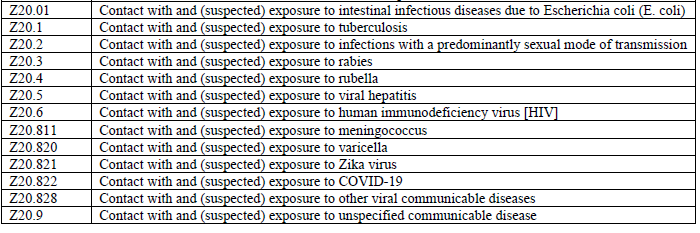
MDC 15: Newborns and Other Neonates: CMS changed newborn encounter coded with a principal diagnosis code from category Z38 (Liveborn infants according to place of birth and type of delivery), followed by codes Z05.1 (Observation and evaluation of newborn for suspected infectious condition ruled out) and Z20.822 (Contact with and (suspected) exposure to COVID-19) from MS-DRG 794 (Neonate with Other Significant Problems) to MS-DRG 795 (Normal Newborn).
Also, took away sdx 13 total contact with and suspected exposure codes in Z20.01-Z20.9 and placed them so they group to MS-DRG 795 as well. These had also been inadvertently left off the grouper logic.
Also added codes P07.0, Extremely low birth weight newborn, unsp weight; P07.20, Extreme immaturity of newborn unsp weight and P07.26, Extreme immaturity newborn gest age 27 weeks to MS-DRG 790 (Extreme Immaturity or Respiratory Distress Syndrome Neonate).
OR to Non-OR and Vice Versa DRG Changes
I will just go over the major changes below.
Procedure codes for embolization of portal or hepatic veins (06L43DZ, 06L83DZ, 06V43DZ, 06V83DZ have been taken out of MS-DRGS 981-983 and now assign to MS-DRGs 423, 424, and 425 (Other Hepatobiliary or Pancreas Procedures with MCC, with CC, and without CC/MCC, respectively).
Excision of hip muscle (biopsy) codes 0KBN3ZX, 0KBN3ZZ, 0KBP3ZX, 0KBP3ZZ with a PDX such as K68.12, psoas abscess taken out of MS-DRGS 981-983 and now assign to 371, 372, and 373 (Major Gastrointestinal Disorders and Peritoneal Infections with MCC, with CC, and without CC/MCC, respectively). NO LONGER OR PROCEDURES!
Other Changes
No changes were made to the Surgical Hierarchies for FY2023.
For Medicare Code Edits (MCE) the additions were self-explanatory and involved new codes for FY2023.
Unspecified Codes: Continuing: Currently there are about 3,490 unspecified codes. Last year in 2021, CMS requested public comments on a potential change to the severity level designations for “unspecified” ICD- 10-CM diagnosis codes that CMS had been considering adopting for FY 2022. Instead, the severity level designations were NOT changed, but a new MCE code edit effective April 1, 2022 would trigger when an “unspecified” laterality diagnosis code currently designated as either a CC or MCC, that includes other codes available in that code subcategory that further specify the anatomic site, is entered. We refer the reader to table 6P.3a of the FY2022 Final Rule which lists unspecified diagnosis codes for laterality that would be subject to this edit. This MCE edit will signal to the provider that a more specific code is available to report. CMS believes this edit aligns with documentation improvement efforts and leverages the specificity within ICD-10. The edit will be 10. Unspecified Code Edit. Payment will not be affected but the claim will be returned for review by the provider. The provider will then need to enter “UNABLE TO DET LAT 1” to identify that they are unable to obtain additional information to specify laterality or they may enter “UNABLE TO DET LAT 2” to identify that the physician is clinically unable to determine laterality.”
For Social Determinants of Health (SDOH) codes, CMS is seeking public comment on whether CMS should consider requiring more robust documentation and claims data reporting to inform the impact on resource use these determinants have on caring for patients affected by these circumstances in an inpatient setting. Also is it thought that homelessness is underreported?
Thus, we are seeking comment on which specific SDOH Z codes are most likely to influence (that is, increase) hospital resource utilization related to inpatient care.
MCC/CC Severity Levels
CMS decided NOT to change any diagnoses on the MCC list or CC list. Only the expanded (new) and other new codes for FY2023 were added. Coders can review tables 6I.1, 6I.2, 6J.1 and 6J.2 for these additions and deletions. For example, M96.A4 Flail chest associated with chest compression and cardiopulmonary resuscitation was added as a new code, and is an MCC. So were several trauma of the brain codes. New code J95.87 for transfusion-associated dyspnea is a CC. See the tables above for a full list.
So there you have it for a summary of the IPPS FY2023 changes. Stay tuned….. In the final Part 4 of this series, the New Technology Add-On Payments (NTAP) will be reviewed in detail.
The information contained in this coding advice is valid at the time of posting. Viewers are encouraged to research subsequent official guidance in the areas associated with the topic as they can change rapidly.
Subscribe to our Newsletter
Recent Blogs
Related blogs from Industry News , Medical Coding Tips
CMS Hospital Compare is a public reporting pl...
Premier benchmarking is widely used by hospit...
PEPPER reports help U.S. hospitals identify o...
CMS has released the updates to the ICD-10-PC...
Subscribe
to our Newsletter
Weekly medical coding tips and coding education delivered directly to your inbox.




