Aug 15, 2022

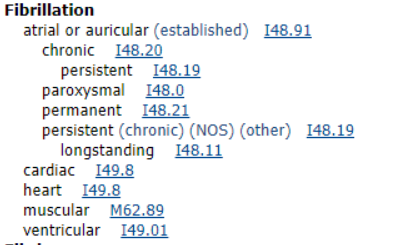
I48.91
used to report atrial fibrillation when no further specificity is available
I48.20
used to report atrial fibrillation when specified as chronic or permanent
I48.19
used to report atrial fibrillation when specified as chronic/persistent
I48.11
used to report atrial fibrillation when specified as persistent/longstanding
I48.0
used to report atrial fibrillation when specified as paroxysmal
I48.21
used to report atrial fibrillation when specified as permanent
What is atrial fibrillation?
Atrial fibrillation is an irregular heartbeat or arrhythmia sometimes called a quivering heart. This arrhythmia can cause a patient to develop blood clots, have a stroke, heart failure or other conditions. The heart rate is most often rapid and causes poor blood flow. When a patient is in atrial fibrillation, the upper chambers of the heart (atria) are beating differently than the lower chambers (ventricles). When this occurs, the irregular rhythm/heartbeat, prohibits the atria from contracting/relaxing and causes ineffectual filling and emptying of the ventricles. This is referred to often as a chaotic dysrhythmia.
The cause of atrial fibrillation is oftentimes unknown but can be the result of damage to the heart’s electrical system caused by conditions such as uncontrolled hypertension and coronary artery disease. Atrial fibrillation can develop in any person including children, but the risk is higher in patients of advanced age, have hypertension, have underlying heart disease, binge drinking of alcoholic beverages, family history, sleep apnea sufferers, athletes, patients with thyroid disease, diabetes and asthma are some of the more common diseases that put a patient at higher risk for developing atrial fibrillation.
Controlling the disease that causes the erratic heartbeat is a must, as well as treating the arrhythmia. Sometimes treating and controlling the underlying cause will make the atrial fibrillation go away. If this does not help the erratic rhythm, then the patient may require treatment with beta blockers and calcium channel blockers to help slow the heart rate. The rhythm should be restored to a normal rhythm to reduce the high heart rate. Patients are often placed on a blood thinner to help prevent blood clot and stroke in addition to the rate and rhythm controller medication. The rhythm should be restored to a normal rhythm to reduce the high heart rate. There are other treatments available such as electrical cardioversion, radiofrequency/catheter ablation, pacemakers and an open-heart maze procedure for the atrial fibrillation that does not correct on its own or does not respond to the medications.
How to code multiple documented types of atrial fibrillation?
The most recent coding advice has addressed how to report the appropriate code for the atrial fibrillation when more than one type is documented. Per this advice, if the physician diagnoses the patient with chronic persistent atrial fibrillation only the code I48.19 (other persistent atrial fibrillation) is reported. The term chronic is a nonspecific term that could also be used to describe the other types of specified atrial fibrillation. Since I48.19 is a more specific code this is the one that should be reported. Even though the Alphabetic Index within ICD-10-CM has listed the different types of atrial fibrillation at the same indention level, only one code is reported. The most specific term should be reported.
Atrial Fibrillation Coding Tips:
- Atrial fibrillation is still reported in patients that are not currently experiencing the erratic rhythm if the patient is requiring ongoing medication to help control the rate
- Atrial fibrillation is very common in postoperative patients and should be verified as a complication before coding as such
- When multiple types of atrial fibrillation are documented in the record select the most specific type
There are other examples of how to code atrial fibrillation when multiple types are documented in the latest issue of Coding Clinic for ICD-10-CM/PCS, Fourth Quarter 2019: Page 7.
Authored by Kim Boy, RHIT, CDIP, CCS, CCS-P
References
heart.org/en/health-topics/atrial-fibrillation/what-is-atrial-fibrillation-afib-or-af
mayoclinic.org/diseases-conditions/atrial-fibrillation/symptoms-causes/syc-20350624
Coding Clinic for ICD-10-CM/PCS, Fourth Quarter 2019: Page 7-8
Coding Clinic for ICD-10-CM/PCS, Second Quarter 2019: Pages 3-4
Coding Clinic for ICD-10-CM/PCS, Third Quarter 2018: Page 6
Coding Clinic, Fourth Quarter 2013 Page: 11 & 98
Coding Clinic, Third Quarter 1995 Page: 8
For the past 30 years, HIA has been the leading provider of compliance audits, coding support services and clinical documentation audit services for hospitals, ambulatory surgery centers, physician groups and other healthcare entities. HIA offers PRN support as well as total outsource support.
The information contained in this coding advice is valid at the time of posting. Viewers are encouraged to research subsequent official guidance in the areas associated with the topic as they can change rapidly.
Subscribe to our Newsletter
Recent Blogs
Related blogs from Medical Coding Tips
CMS Hospital Compare is a public reporting pl...
Premier benchmarking is widely used by hospit...
PEPPER reports help U.S. hospitals identify o...
CMS has released the updates to the ICD-10-PC...
Subscribe
to our Newsletter
Weekly medical coding tips and coding education delivered directly to your inbox.