
Recrudescence of stroke, also called stroke mimic, is the temporary return of neurological deficits that have previously resolved, in the absence of new damage/stroke, in a patient with an earlier cerebral infarction.
Causes of Recrudescence
Temporary return of neurological deficits can occur anytime, even years after they previously resolved. Recrudescence occurs in approximately 10% of patients with transient neurological issues, is usually mild and lasts less than 24 hours. There are several conditions that can trigger an episode of recrudescence, including:
- Infection
- Hypotension
- Hyponatremia
- Insomnia
- Stress
- Use of benzodiazepines
- Dehydration
- Overexertion
Recrudescence vs. Relapse
While recrudescence indicates a temporary return of symptoms, relapse is the recurrence or worsening of symptoms after a period of relief. This can be an indicator of new or progressing infarction. The key to an episode of recrudescence is no new damage or extension of previous area of infarction. If the documentation is unclear, query the provider to determine if the return of symptoms is temporary or due to progression of a previous stroke or an altogether new stroke.
ICD-10-CM Coding
Clear documentation of the underlying cause of the neurological deficits will be necessary to decipher between recrudescence, relapse or a new stroke. However, once it’s been established that the patient’s symptoms are temporary and not due to a new cerebral infarction the diagnosis coding is as easy as following the terms in the Alphabetic Index.
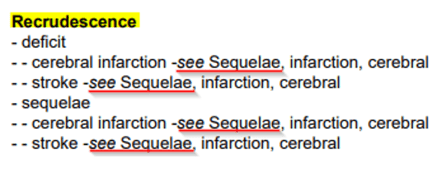
Alphabetic Index
It’s clear from the direction in the index that recrudescence of a previous stroke is coded as a sequela of the previous cerebral infarction.
The direction in the index is supported by official advice in AHA Coding Clinic which says, “…it is appropriate to assign sequela(e) codes for conditions documented as due to recrudescence of a stroke.”
Coding Guideline
ICD-10-CM coding guideline I.C.9.d.1 directs how to code neurologic deficits that are sequelae of a cerebral infarction. In summary, the guideline directs
- Codes for sequelae of cerebrovascular disease are assigned from category I69 Sequelae of cerebrovascular disease
- The neurologic deficits caused by cerebrovascular disease may be present from the onset or may arise at any time after the onset of the acute infarction
- Codes from category I69, Sequelae of cerebrovascular disease, that specify hemiplegia, hemiparesis and monoplegia identify whether the dominant or nondominant side is affected.
- Should the affected side be documented, but not specified as dominant or nondominant, and the classification system does not indicate a default, code selection is as follows:
- For ambidextrous patients, the default should be dominant.
- If the left side is affected, the default is non-dominant.
- If the right side is affected, the default is dominant.
Example:
Mr. Evans, a 73 yr. old male patient, presents to the Emergency Department secondary to left sided facial weakness and weakness of left arm similar to what he experienced when he had a cerebral infarction 18 months ago. He states that he has been under a lot of stress lately and has had trouble sleeping. Radiologic imaging shows an area of previous infarction, but no current pathology. The final diagnosis is transient facial weakness and monoplegia secondary to previous stroke, no evidence of new or worsening infarction.
ICD-10-CM Diagnosis Codes:
- I69.334 Monoplegia of upper limb following cerebral infarction affecting left non-dominant side
- I69.392 Facial weakness following cerebral infarction
Take Aways
- Recrudescence of stroke is the temporary return of neurological deficits related to a previous cerebral infarction without the presence of new damage/stroke.
- Clear documentation is essential in determining whether a patient has recrudescence of stroke, relapse of stroke or new stroke.
- Recrudescence of stroke is coded as sequelae of stroke with codes from category I69.
- Follow the direction in ICD-10-CM coding guideline I.C.9.d.1 for specific guidance in assigning codes for sequelae of cerebral infarction.
For more detailed information about coding for cerebral infarctions, take our HIALearn course Cerebrovascular Accident Infarction Thrombosis and Embolus or Stroke and Sequelae Coding.
References
FY 2025 ICD-10-CM Alphabetic Index
Coding Clinic for ICD-10-CM/PCS, Second Quarter 2024, Page 13
https://www.healthline.com/health/stroke/recrudescence-stroke
Since 1992, HIA has been the leading provider of compliance audits, coding support services and clinical documentation audit services for hospitals, ambulatory surgery centers, physician groups and other healthcare entities. HIA offers PRN support as well as total outsource support.
The information contained in this coding advice is valid at the time of posting. Viewers are encouraged to research subsequent official guidance in the areas associated with the topic as they can change rapidly.
Subscribe to our Newsletter
Recent Blogs
Related blogs from Industry News , Medical Coding Tips
CMS Hospital Compare is a public reporting pl...
Premier benchmarking is widely used by hospit...
PEPPER reports help U.S. hospitals identify o...
CMS has released the updates to the ICD-10-PC...
Subscribe
to our Newsletter
Weekly medical coding tips and coding education delivered directly to your inbox.

.png)


