A higher CMI corresponds to increased consumption of resources and increased cost of patient care, resulting in increased reimbursement to the facility from government and private payers, like CMS.
We know that documentation directly impacts coding. Therefore, if a physician does not document all the services the patient received or if the coding is not accurate, the result could be undercoding, lowering your overall CMI and leaving revenue on the table.
Look at the example below to see how HIA’s findings impacted our client’s CMI.
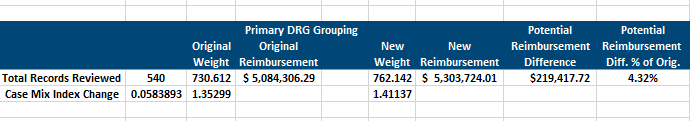
Overall Potential Reimbursement Impact: Potential increase of $2,552,125.32 when extrapolated across the 2018 inpatient discharges (using 6,282 as annual number of accounts). CMI based on accounts reviewed not overall casemix. Reimbursment based on $6,958.97 facility base rate.
Ensure the health of your facility’s CMI by scheduling regular coding audits with HIA.




