
Medicare Advantage Plans (Medicare part C) use risk adjustment payment to calculate reimbursement for care provided to a Medicare Advantage beneficiary.
Why Risk Adjustment?
Individuals with severe or chronic conditions that require ongoing management typically require greater amounts of care that must be paid for by their insurance plan. In some cases, the cost of care could even exceed the premiums collected from that beneficiary. The costliness of their care makes these patients high risk. Risk adjusted payment models seek to adjust the burden of risk to be shared by all insurers and allowing them to cover high risk individuals for the same premiums as low risk individuals.
Risk adjusted payment models classify those who are high risk by identifying an individual’s chronic and severe conditions to build a health profile called a “base year” and then translating that information into a risk adjustment factor (RAF) score or risk score.
Risk Adjustment and HCCs
Medicare uses the hierarchical condition categories or HCC model to calculate payment for the Medicare Advantage plan. This model assigns diagnoses to one of 115 HCCs that are organized into 26 disease groups representing clinically related conditions with similar cost patterns.
It's important to note that not every diagnosis is assigned to an HCC. Typically, chronic conditions such as diabetes, COPD, or CHF “risk adjust” or map to an HCC. With a few exceptions, injuries and acute illnesses do not map to an HCC because they are not good predictors of long-term health care costs.
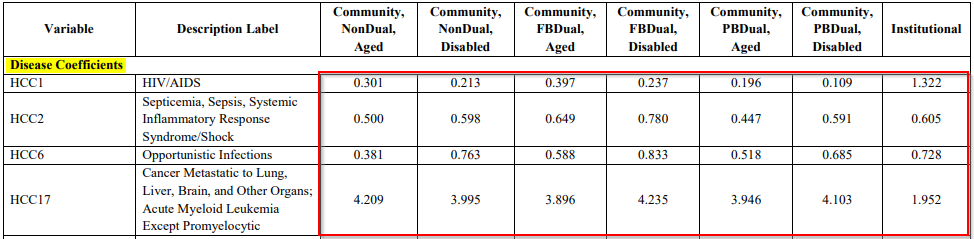
Each HCC has corresponding coefficients that are used in the calculation of the risk score. The value of the coefficient for an HCC may differ depending on specific characteristics of the patient such as age, disability status, whether the patient is dually eligible (eligible for both Medicare and Medicaid), and whether the patient lives in the community or an institution.
Example:
Under the HCC model, providers treating Medicare Advantage plan patients are paid based on the patient’s risk score. Through the assignment of HCCs, payment is calculated based on what it will take to manage the patient’s severe and chronic conditions during the next year, not by how often they see the patient. In this way HCC is a prospective payment model, similar in many ways to the DRG system used for inpatient admissions, because it uses the diagnoses in a patient’s health file to determine a comprehensive amount to be paid to the provider for managing the patient’s severe and chronic conditions over the next year.
ICD-10-CM Coding for HCCs
Documentation from which diagnoses assigned to an HCC are generated must result from a face-to-face visit between the patient and the provider and assignment of HCCs must be made based on ICD-10-CM codes assigned according to ICD-10-CM guidelines.
Since this is the case, comprehensive documentation and correct coding are critical to painting an accurate clinical picture that translates into appropriate reimbursement. When diagnoses or specificity are missed due to incomplete documentation or improper coding the provider may receive payment that does not accurately reflect the complexity of managing the patient’s care.
What is M.E.A.T.?
To support the mapping of a diagnosis to an HCC, the documentation must support the presence of the disease or condition and how the provider assessed and/or plans to manage the problem. To ensure that documentation supports the coding that HCC assignment is be based on, include M.E.A.T. in the documentation.
M.E.A.T. stands for monitor, evaluate, assess and treat.
| M.E.A.T. | |
| Monitoring | Documentation of monitoring signs, symptoms, syndromes, disease progression/regression, ongoing surveillance. |
| Evaluation | Documentation of evaluating test results, medication effectiveness and response to treatment. Documentation of physical evaluation. |
| Assessing | Documentation of diagnostic tests, counseling, review of records, discussion of chronic condition(s). |
| Treating | Documentation of prescribing or managing medication, ordering therapies, procedures or other modalities/treatments, making referrals and documentation of plans for ongoing or future management of chronic conditions. |
Example
The patient has Type 2 diabetes mellitus on 0.5 units of Lantus daily. Blood sugar not well controlled on current dosage. Blood sugar reading is 250. Increase dosage to 1 unit of Lantus daily.
Take Aways
When coding for patients whose care will be reimbursed under the HCC risk adjusted payment model, the annual reimbursement for that patient is dependent on complete and accurate assignment of ICD-10-CM codes at the highest degree of specificity. To generate documentation that supports optimal diagnosis coding be sure the documentation includes the elements of M.E.A.T., monitoring, evaluation, assessment and treatment.
For more information on the HCC reimbursement methodology, read Hierarchical Condition Categories (HCCs), Release of Model V28.
References
https://www.cms.gov/priorities/innovation/key-concepts/risk-adjustment https://www.cms.gov/medicare/health-plans/medicareadvtgspecratestats/risk-adjustors/2024-model-software/icd-10-mappings
Since 1992, HIA has been the leading provider of compliance audits, coding support services and clinical documentation audit services for hospitals, ambulatory surgery centers, physician groups and other healthcare entities. HIA offers PRN support as well as total outsource support.
Subscribe to our Newsletter
Recent Blogs
Related blogs from Industry News , Medical Coding Tips
CMS Hospital Compare is a public reporting pl...
Premier benchmarking is widely used by hospit...
PEPPER reports help U.S. hospitals identify o...
CMS has released the updates to the ICD-10-PC...
Subscribe
to our Newsletter
Weekly medical coding tips and coding education delivered directly to your inbox.


.png)


