ICD-10 Implementation
The infamous ICD-10 transition was compared to Y2K with over-hyped catastrophic consequences that ultimately fell flat. It took over 20 years and 3 delays before finally being implemented. Opponents to ICD-10 claimed that hospitals would be negatively impacted. They predicted a major drop in coder productivity, that would slow down payments and cause business disruption. While ICD-10 proponents highlighted the policy issues. Wacky ICD-10 codes like being struck by an orca or having problems with relationships with in-laws were mocked and used as an example of the government demanding too much detail, creating an unnecessary burden for providers. However, the transition to ICD-10 turned out to be a smooth process.
At HIA, we saw minimal downtime, and coder productivity and quality weren’t significantly compromised. We ran accuracy rates for all inpatient coders in January of 2015 and January of 2016 (after the implementation of ICD-10). We saw an increase in Total DRG accuracy from 93.16% to 94.74% and an increase in Total Codes accuracy from 93.27% to 93.47%. So, like Y2K, the ICD-10 transition was a nonevent. None of the dire predictions have come true and the healthcare industry has moved on.
ICD-10 implementation timeline within the past decade:
2010
CMS institutes a code freeze in preparation for ICD-10. I
2012
Facing backlash from physicians’ groups, HHS publishes a final rule that delays the compliance date for ICD-10-CM/PCS from October 1, 2013 to October 1, 2014.
April 2014
The Protecting Access to Medicare Act of 2014 is enacted, which contains a provision prohibiting the HHS Secretary from adopting the
ICD-10 code prior to October 1, 2015.
January 2015
CMS begins end to end testing of ICD-10.
October 2015
ICD-10-CM/PCS implementation deadline.
Source
http://library.ahima.org/doc?oid=107657#.XhXuDhdKh0s
http://library.ahima.org/doc?oid=301834#.XhXyoxdKh0s
Code Changes
That’s a 379.3% increase in ICD-10-CM codes and a 1,754% increase in ICD-10-PCS codes!
So just what are all these new codes? Well, ICD-10 was developed to accommodate new diagnosis and procedure codes for future clinical protocols that can improve quality measurements, patient safety, and evaluation of medical processes and outcomes.
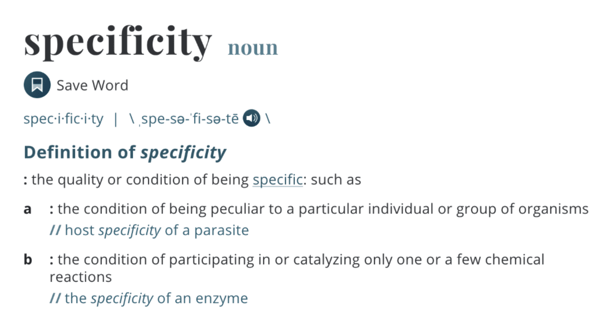
In other words, it all centers around one word: specificity.
Following 2015, both ICD-10-CM codes and ICD-10-PCS codes only saw marginal increases, with diagnoses codes increasing 3.38% and procedure codes increasing 7.76%.
DRG’s stayed pretty consistent throughout the 2010’s, with only a 2% increase since the start of the decade.
CPT codes also didn’t see too much of a change – from 2010 to 2020, there was only a 14.87% increase.
Acute/Profee Timeline
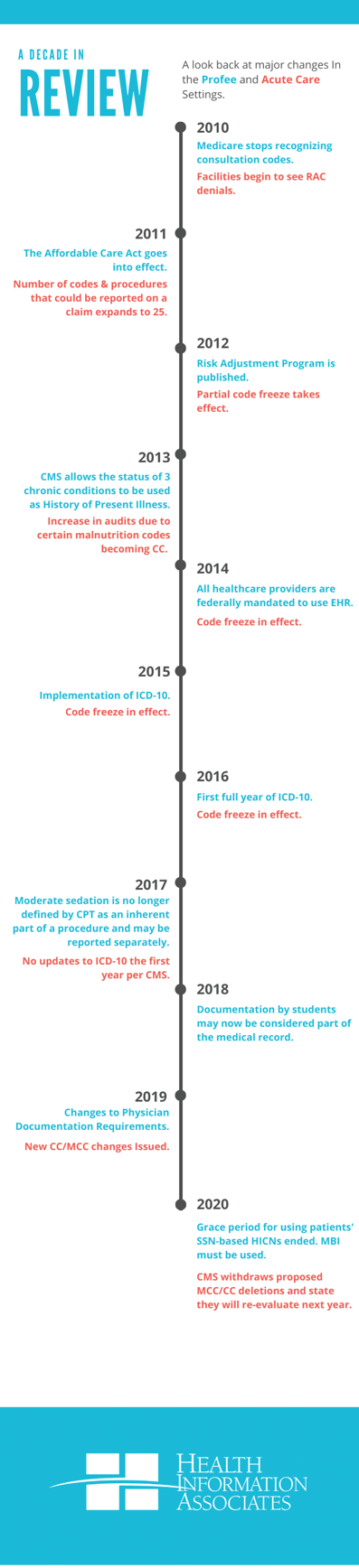
RAC Timeline
The goals of the RAC program include:
- Detecting and correcting past improper payments so CMS may implement actions to prevent future improper Medicare payments
- Identifying areas of provider confusion within Medicare billing
- Assisting CMS in addressing the high error rate within Medicare – currently 11% which equates to a loss of $41 billion per year
- Helping to maintain the future solvency of the Medicare Trust Fund for the millions of seniors who rely on the program
Who is subject to a RAC Audit?
- Hospitals
- Physician practices.
- Nursing homes.
- Home health agencies.
- Durable medical equipment suppliers.
- Any provider or supplier that submits claims to Medicare.
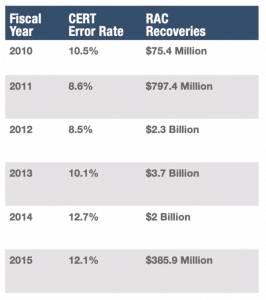
Below is an overview of the RAC recoveries since 2010 and the Medicare billing error rate (CERT).
The American Hospital Association (AHA) filed a suit in 2014 to try and clear a backlog of RAC appeals at the administrative law court level. There were at least 800,000 appeals at that level as of 2014. A lower federal court had dismissed the lawsuit due to lack of jurisdiction, concluding because Congress was working on trying to procure more funding to review claims, it did not yet have the authority to act further. However, the case was reinstated by an appeals court.
The AHA notes that in December 2013, with the large backlog of appeals mounting, HHS imposed a two-year moratorium on assigning new appeals of claim denials. The court’s opinion observed that the department “has the capacity to process only about 72,000 appeals per year, a far cry from the almost 400,000 appeals it received in fiscal year 2013, or from the more than 800,000 appeals that composed its backlog in July 2014. These figures suggest that at current rates, some already filed claims could take a decade or more to resolve.” That administrative logjam delays billions of dollars in Medicare reimbursements to hospitals, the AHA noted.
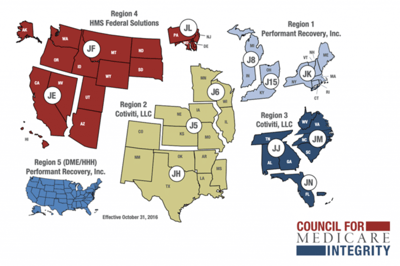
On October 31, 2016, CMS announced the next round of RAC contracts had been awarded.
Five new contracts have been awarded – four regional contracts and one for a new region focused solely on auditing DME/HH-H claims nationwide. RACs in Regions 1-4 will conduct post-payment reviews to identify improper payments made in Parts A and B, excluding Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) and Home Health/Hospice (HH-H) providers. The RAC in the newest region, Region 5, will conduct post-payment reviews on DMEPOS and HH-H nationwide.
The map below illustrates the different regions that are covered by these contracts.
For most practices, the best defense against RAC is an effective offense. The best way to verify you are in compliance is to schedule frequent external audits (coding reviews). By doing so, you can uncover any issues and put corrective action in place, so the issue doesn’t continue (and you won’t be forced to pay back the government!).
Ransomware
| Year Reported to HHS | Number of Hacking Events Reported | Number of Patients Affected by Hacking Events |
| 2010 | 10 | 568,358 |
| 2011 | 16 | 297,269 |
| 2012 | 16 | 900,684 |
| 2013 | 19 | 206,998 |
| 2014 | 31 | 1,786,630 |
| 2015 | 34 | 93,227,349 |
Source: US Department of Health and Human Services Office for Civil Rights. “Breach Portal: Notice to the Secretary of HHS Breach of Unsecured Protected Health Information.” June 30, 2015. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf.
The main takeaway is that HIM professionals must remain vigilant in protecting an organization from internal and external threats. Threats are continually evolving, therefore, solutions to protect information must remain one step ahead. Hackers and cyber-attackers only need to get it right once. Healthcare organizations have to get it right every day. One weak link is all it takes for a hacker to get in.
Meaningful Use
The main EHR features required to fulfill HITECH meaningful use requirements are:
- A core of consistent, structured, clinical content that would be uniform across vendor systems and care settings
- Automated alerts and reminders
- Consistent, robust measurement capabilities
- Data mining capabilities
- Public health reporting
- Interoperability with other systems
What’s Next? A Look Ahead
ICD-11 will be the next hurdle for our industry to panic over and, ultimately, over-prepare for. The new classification system is set to take effect January 2022, but if ICD-10‘s implementation is any indication, this date is just a ballpark timeframe. ICD-11 is promised to be a vast improvement on the previous revisions, considering critical advances in science and medicine, while aligning classification with the latest knowledge of disease treatment and prevention. A significant feature is the improved ease and accuracy of coding requiring less user training than before. It will also have a translation tool to ensure internally consistent translations, including locally used terms. To learn more about ICD-11 view: https://icd.who.int/en/docs/icd11factsheet_en.pdf
Merit-Based Incentive Payment System (MIPS)
Under MIPS, there are 4 performance categories that could affect your future Medicare payments. Each performance category is scored by itself and has a specific weight that is part of the MIPS Final Score. The payment adjustment determined for each MIPS eligible clinician is based on the Final Score. These were the performance category weights for the 2019 MIPS Performance Year:
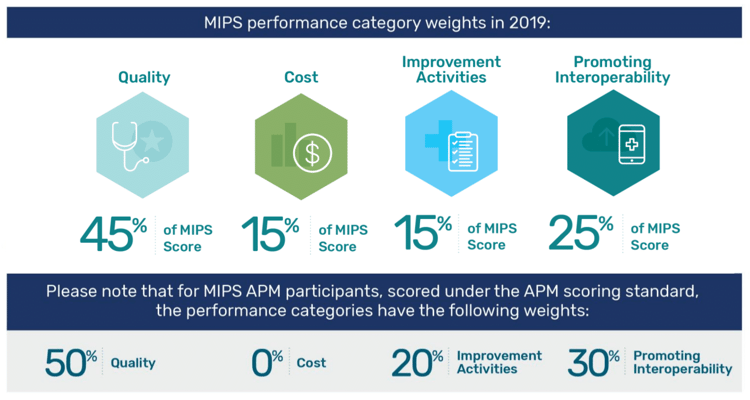
Graphic courtesy qpp.cms.gov
For 2020, the scoring will remain the same. However, in 2021, the scoring will be 35% Quality, 25% Cost, 25% Promoting Interoperability, and 15% Improvement Activities.
For 2022, the scoring will be 30% Quality, 30% Cost, 25% Promoting Interoperability, and 15% Improvement Activities.