Feb 13, 2024
In recent audit cases, HIA has seen coders missing the coding of a phlegmon that is documented by the physician. In some cases, the coding can impact the DRG or APR SOI/ROM as it in many cases is coded as an MCC.
What is a phlegmon?
A phlegmon is a localized area of acute inflammation of the soft tissues. It is a descriptive term which may be used for inflammation related to a bacterial infection or non-infectious causes (e.g. pancreatitis). A phlegmon is unlimited and can continue to spread through connective tissue and muscle fibers. In some cases, it can be difficult to distinguish an abscess from a phlegmon. Sometimes phlegmon occurs when infected material inside an abscess ruptures and spreads.
Coding of Phlegmon is an MCC and Impacts APR SOI/ROM
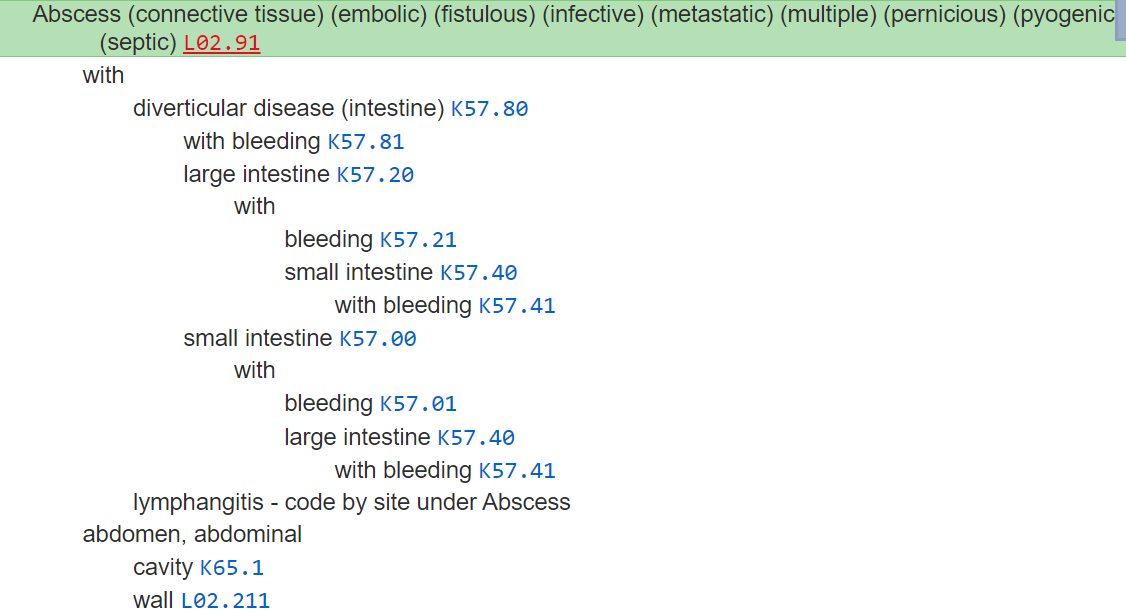
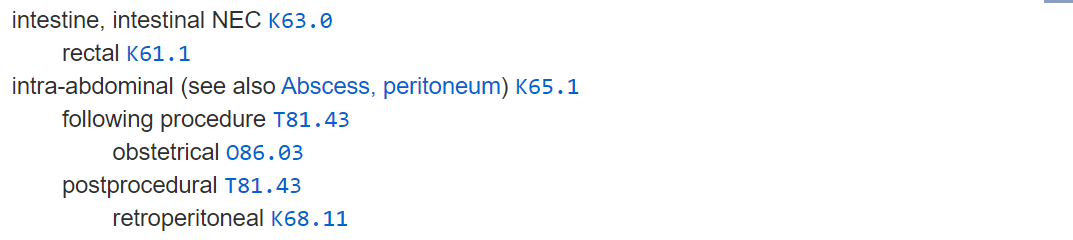
The coder may think that a phlegmon is not necessary to code. Or may not even look at the index or place the diagnosis in the encoder. However, if one looks in the index, it shows:
Phlegmon - see Abscess
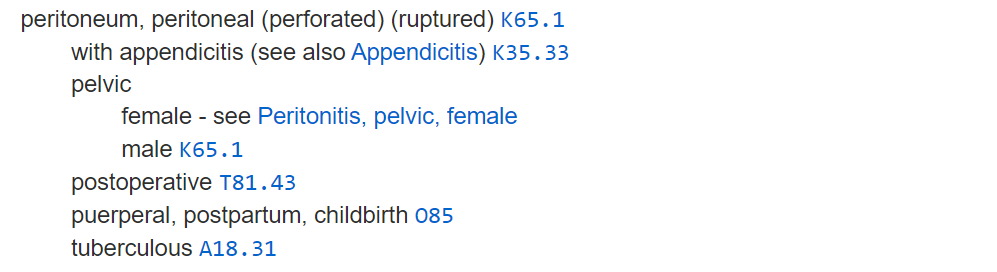
The coder then must look for the location of the abscess. For example, if the abscess is intraabdominal, or in the abdominal cavity code K65.1 is assigned. If it is associated with diverticulosis or diverticulitis, a code K57.- would be assigned. In addition there is a code also note under this category.
Phlegmon Example
In this case the auditor added secondary diagnosis K65.1 (Peritoneal abscess) for the phlegmon. This will shift the DRG from 331 Major small and large bowel procedures without CC/MCC to 329 Major small and large bowel procedures with MCC and affects the APR DRG SOI 2 to SOI 3.
This 43 y/o male presents with abdominal pain. CT abdomen pelvis with and free air under diaphragm, peritoneal cavity phlegmon measuring up to 6 cm in size, as well as scattered free fluid in the anterior pelvis. Surgery consulted, taken to OR tonight, underwent ex lap, sigmoid colectomy, colostomy (Hartman's procedure). Intraoperatively, found to have large amount of purulent fluid throughout the entire abdomen with inflamed colon.
CT: “PERITONEAL CAVITY: Pericolonic air as well as scattered free air in the abdomen and under the hemidiaphragm consistent with perforation. There is an amorphous soft tissue region in the peritoneal cavity measuring up to 6 cm in size at the level of L5. Contains small amounts of air. Finding presumably represents infectious phlegmon of the mesentery/peritoneal cavity. Scattered areas of free fluid in the pelvis. ABDOMINAL WALL: Unremarkable. LOWER THORACIC: No effusion. OSSEOUS: Unremarkable. IMPRESSION: 1. Extensive severe acute sigmoid diverticulitis with perforation and free air under the diaphragm. 2. Peritoneal cavity phlegmon as described above. 3. Some free fluid noted in the anterior pelvis.
FINAL REPORT Attending MD Date Signed Off
History of Present Illness
43 y.o. Male with no significant PMH presented in ER with abdominal pain. CT abdomen pelvis with extensive severe acute sigmoid diverticulitis with perforation and free air under diaphragm, peritoneal cavity phlegmon measuring up to 6 cm in size, as well as scattered free fluid in the anterior pelvis. Surgery consulted, taken to OR tonight, underwent ex lap, sigmoid colectomy, colostomy. Intraoperatively, found to have large amount of purulent fluid throughout the entire abdomen with inflamed colon.
- # Perforated diverticulitis
- # Peritoneal cavity phlegmon
- # S/p ex lap, sigmoid colectomy, sigmoid colostomy
-Patient was taken to the OR, intraoperatively found to sigmoid tumor and have large amount of purulent fluid in abdomen with inflamed phlegmon, underwent ex lap, sigmoid colectomy, colostomy.
-Diet, pain medications, VTE prophylaxis per surgery
-Continue Zosyn
OPERATIVE NOTE ABBREVIATED:
EXPLORATORY LAPAROTOMY, Sigmoid colectomy, Colostomy
Surgical Findings: __Purulence present at time of surgery. _Location: Organ Space_. __
Inflamed sigmoid colon with purulence throughout the abdomen
Anesthesia: General
Specimen:
ID Type Source Tests Collected by Time
1 : sigmoid colon Tissue Abdomen SURGICAL PATHOLOGY
A : abdominal fluid Body Fluid Abdomen CULTURE: AEROBIC AND ANAEROBIC W/GRAM STAIN - WOUND (OTHER)
“…..A large amount of purulent fluid was encountered throughout the entire abdomen. Cultures were taken. Several hundred cc of purulent fluid was suctioned from the abdomen. There was significant inflammation of the sigmoid colon. It was hard and fixated in place. It was noted that there was phlegmon and pockets of fluid throughout the abdomen, in the pelvis, above the liver, in the gutters and between loops of bowel, consistent with the history of perforated viscus. Small bowel loops were eviscerated in order to examine the bowel…..
…… Attention was turned to the sigmoid colon. A window was created in the mesentery using electrocautery at a site proximal to the thickened area. A blue load of the GIA stapler was used to divide the bowel proximal to the thickened area. LigaSure was used to divide the mesentery to a site beyond the perforation. The mesentery was divided to the level of the colon at the sacral promontory where the rectum was soft and healthy. A curved contour stapler was used to the divide the colon as this site. Once freed, the colon was passed off the field and submitted to pathology. The rectal stump was marked with two Prolene sutures for future re-anastomosis……
……. A site just left of midline was selected for creation of an ostomy. The electrocautery was used to excise a circle of skin and then dissect out a core of subcutaneous tissue down to the level of the fascia. The fascia was opened in a cruciate fashion. The rectus muscle was spread, and the posterior sheath and peritoneum were grasped and elevated. This was similarly incised in a cruciate manner, ensuring no bowel was injured below.
The proximal colon was mobilized by incising the white line of Toldt until an adequate length of colon was able to brought to the abdominal wall. A Babcock was used to grasp a staple line on the bowel and bring it through the hole in the fascia.”
In the above case, principal diagnosis was coded as K57.20, Diverticulitis of large intestine with perforation and abscess without bleeding along with the procedures below. The DRG assigned was 331 - Major small and large bowel procedures without CC/MCC. By following tabular code also note and Coding Clinic advice and adding the K65.1 for the abscess, the DRG changes to 329 - Major small and large bowel procedures with MCC.
0DBN0ZZ Excision of Sigmoid Colon, Open Approach
0D1N0Z4 Bypass Sigmoid Colon to Cutaneous, Open Approach
Refer to the Alphabetic Index which shows that phlegmon is coded as "abscess". Refer to Tabular Instruction of K57- which states to “Code Also, if applicable, peritonitis (K65.-).” Refer to Coding Clinic: Diverticulitis with Intra-Abdominal Abscess Coding Clinic for ICD-10-CM/PCS, First Quarter 2022: Page 26 that supports coding peritonitis or intra-abdominal abscess, K65.1 in addition to the code of diverticulitis with perforation and abscess.
References
Coding Clinic First Quarter 2022, page 26
Official Guidelines for Coding and Reporting
Health Information Associates offers medical coding services, medical auditing services, and clinical documentation audit services for hospitals, ambulatory surgery centers, physician groups and other healthcare entities in the United States.
The information contained in this coding advice is valid at the time of posting. Viewers are encouraged to research subsequent official guidance in the areas associated with the topic as they can change rapidly.
Subscribe to our Newsletter
Recent Blogs
Related blogs from Medical Coding Tips
CMS Hospital Compare is a public reporting pl...
Premier benchmarking is widely used by hospit...
PEPPER reports help U.S. hospitals identify o...
CMS has released the updates to the ICD-10-PC...
Subscribe
to our Newsletter
Weekly medical coding tips and coding education delivered directly to your inbox.




